(USMLE topics) Calcium metabolism and hypocalcemia: causes, symptoms, pathology, treatment. This video is available for instant download licensing here : https://www.alilamedicalmedia.com/-/galleries/narrated-videos-by-topics/electrolyte-acid-base-balance/-/medias/33d05c38-58ef-4d48-8ab8-654155fc3c84-hypocalcemia-narrated-animation
©Alila Medical Media. All rights reserved.
Voice by: Ashley Fleming
Support us on Patreon and get FREE downloads and other great rewards: patreon.com/AlilaMedicalMedia
All images/videos by Alila Medical Media are for information purposes ONLY and are NOT intended to replace professional medical advice, diagnosis or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition.
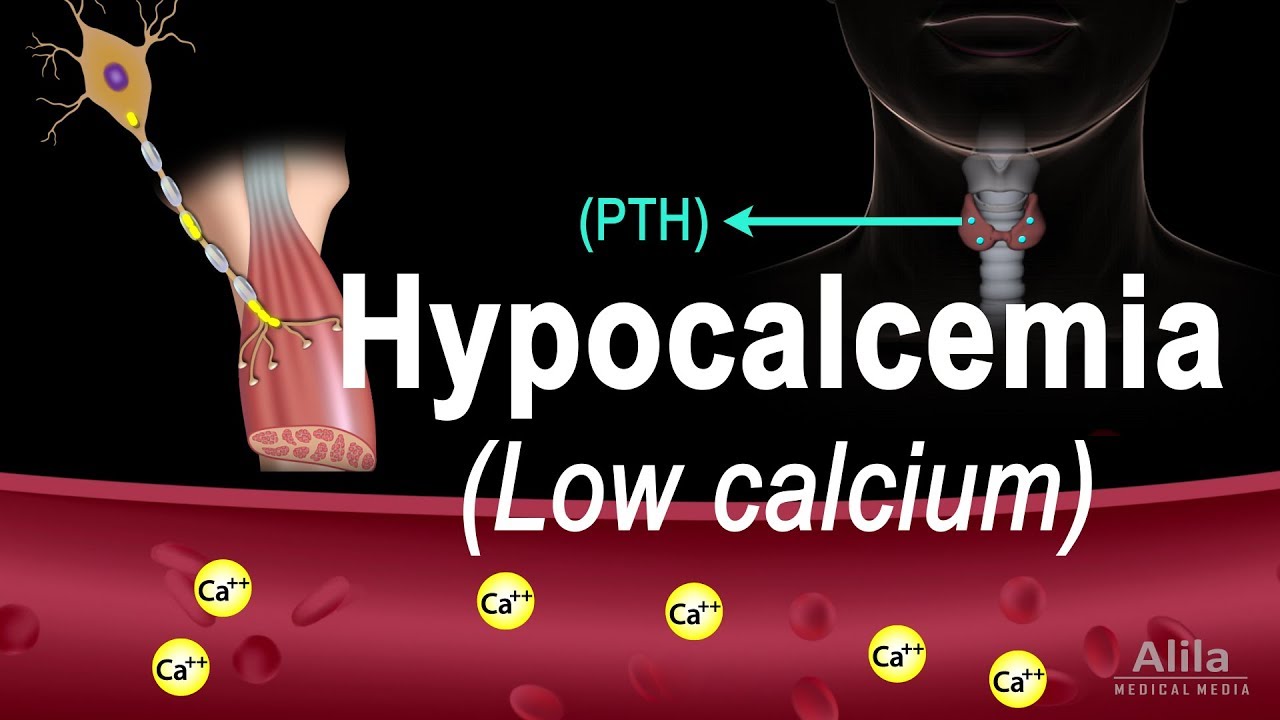
In the body, most calcium is located in bones, only about 1% is in the blood and extracellular fluid. The amount of calcium in circulation is regulated by 2 hormones: parathyroid hormone, PTH, and calcitriol. When serum calcium level is low, PTH is UPregulated. PTH acts to PROMOTE calcium release from bones and REDUCE calcium loss from urine. At the same time, it stimulates production of calcitriol, which promotes absorption of calcium in the small intestine while also INcreases RE-absorption in the kidney. Together, they bring UP calcium levels back to normal. The REVERSE happens when calcium level is high. This feedback loop keeps serum calcium concentrations within the normal range.
HYPOcalcemia refers to ABnormally LOW levels of calcium in the blood and is generally defined as serum calcium level LOWER than 2.1 mmol/L. Because the total serum calcium includes albumin-bound and free-ionized calcium, of which only the LATTER is physiologically active, calcium levels must be corrected to account for albumin changes. For example, DEcreased albumin levels, such as in liver diseases, nephrotic syndrome, or malnutrition, produce LOWER serum calcium values but the amount of FREE calcium may STILL be normal. On the other hand, in conditions with high blood pH, albumin binds MORE calcium; leaving LESS FREE-ionized calcium in the serum while the total calcium level may appear normal.
The most common cause of hypocalcemia is PTH deficiency resulting from DEcreased function of the parathyroid glands, or HYPOparathyroidism. HYPOparathyroidism, in turn, may be caused by a variety of diseases and factors. These include:
– accidental removal or damage of the parathyroid glands during a surgery
– autoimmune disorders
– congenital disorders: mutations that set the “normal calcium levels” to a lower value
– other genetic disorders that produce underdeveloped or non-functional parathyroid glands
– magnesium deficiency
Other causes of hypocalcemia include low vitamin D intake/production, and excessive loss of calcium from the circulation such as in kidney diseases, tissue injuries or gastrointestinal diseases.
While chronic moderate hypocalcemia may be Asymptomatic, ACUTE and severe hypocalcemia can be life-threatening. Most symptoms of acute hypocalcemia can be attributed to the effect it has on action potential generation in neurons. Because extracellular calcium INHIBITS sodium channels, and consequently DEpolarization, REDUCED calcium level makes it EASIER for depolarization to occur. Hypocalcemia therefore INCREASES neuronal excitability, causing neuromuscular irritability and muscle spasms. Early symptoms often include numbness and tingling sensations around the mouth, in the fingers and toes. As the disease progresses, muscle spasms may manifest as tetany, wheezing, voice change, and dysphagia. Seizures may occur in severe cases. Effects of hypocalcemia on cardiac function include long QT interval due to prolonged ST fragment, congestive heart failure and hypotension.
Acute hypocalcemia should be treated promptly with intravenous calcium. Chronic hypocalcemia is usually treated with oral calcium and possibly vitamin D supplementation.
source